Title: My Father’s Paradise by Ariel Sabar
Subtitle: A Son’s Search for His Family’s Past
Why: A co-worker recommended it, and is related to the author, thus making the book a family history for him (how cool is that!)
Review:
I learned a lot of history that I sadly had been clueless about before reading this book. I never knew that there was a significant Jewish population in Iraq, nor that they lived relatively harmoniously with Muslims and Christians there for hundreds of years. I didn’t know about the semi-forced migration of Jews from Arab countries to the newly formed Israel after World War II and the dire circumstances surrounding such migration. I didn’t know that there was a social hierarchy between European/Ashkenazi Jews and Arabic Jews, and another hierarchy with Arab Jews depending on if you were Baghdadi or Kurdish, for example. The story is written by a 50-ish year old journalist who investigates his family history starting with his great grandfather in Kurdistan (Iraq). It details the forced migration that his father endured from Iraq to Israel at the age of 13, and all of the struggles that come from coming of age in a new strange place. Eventually it continues to his father’s migration to the US, and to the author being born and turning into the most annoying teenage rebel, wanting nothing to do with his family’s heritage. And then, of course, that rebel grows up, sees the error of his ways and then uses his newfound journalistic skills to turn his families stories into a proper history.
The book is very well written and engages you from beginning to end. This is not a textbook, but rather a fireside story. I was furious at the childishness of the author for rebelling against his parents in such a disrespectful way, but I think most of my fury was actually directed at myself for having similar tendencies and feelings, though I kept them mostly bottled up inside of me. I identified strongly with the immigrant story as it is nearly identical to mine, though my parents came from a different country and were fortunate to make the choice to leave their homeland willingly. But I know they suffered mightily to do so, leaving one home, and landing in a place that never could be anything but a second home, one that doesn’t quite ever feel like home.
This quote could have been written about my childhood:
My father would hand me the phone on my visits home to Los Angeles, and I would listen as a stream of Aramaic blessings crossed ten time zones along a crackling telephone line. My father would pass me the receiver and whispher, “Just say amen every so often. It will make her feel good.” I said my amens and returned to my life.
I’m envious and impressed by Sabar’s work in documenting his family history, as I have never taken the time or energy to do anything similar with my own. I’m now an American through and through, and I’m OK with that, but I wish I could have passed more appreciation of our culture on to my kids. Hopefully they will eventually get curious and learn on their own, but more likely I’ve just accelerated a path to distancing future generations from our homeland. Anyways, that is all a digression from the story, though to be honest, it is the central tenet of the book. I’m really glad that I read this one.
Title: CivilWarLand in Bad Decline by George Saunders
Why: A co-worker recommended and I vaguely remember liking Lincoln in the Bardo
Review:
It is a series of short stories, all with the thread of being set in various near-future dystopias with flawed characters. It’s definitely on the weird/absurd side of things. Parts of it reminded me of The Stand or Station 11, two books I really liked. Parts were humorous and parts were absolutely disgusting, but throughout, it shed a light on human nature, even in those weird circumstances. I wouldn’t read it again, but I’m glad it and I added Pastoralia to my to-read list.
Title: Choosing To Run by Des Linden
Why: It’s a running book and who isn’t inspired by Des Linden?
Review:
This autobiography was a page turner that I read during a car ride back from Florida. (Don’t worry, I wasn’t driving). I’m a sucker for running books and this was a great one, mostly because Des Linden is so down-to-earth that you just want to root for her through every obstacle. I also love what a vivid, detailed memory she has of her races. It allowed me to go back to watch the 2018 Boston marathon videos, in particular, and feel like I was in her mind, and in the mind of the runners around her.
I was a bit confused initially by the alternating chapter approach, but it build up suspense about her 2018 performance, which I guess was the point. As a doctor, I was frustrated with her for ignoring the straightforward medical advice that she was getting, though it is understandable given her situation, and her concerns about doping in sports. And to her credit, she researched her conditions thoroughly and made the right decisions. As I was reading her symptoms I immediately wondered if she was hypothyroid, and now I wonder if she actually had burned-out Graves, with her mild exopthalmos. Anyway, enough pop-diagnosis. The book is excellent and I would read more by her if she ever writes another book.
Favorite quote from the book:
“The grind” meant something positive to me: a challenge to embrace repetition and approach it creatively. It annoyed me when I heard “the grind” used in a pejorative way. Sure, it could be tedious, but it was a choice. Go off and do something else if you hate it.
Preach!
-
Old people can build muscle. Sorry,
this one is behind a paywall, but it basically describes a study that showed that muscle
SFI decreased in old people (ages 60-79) with resistance training. Muscle SFI (shape
factor index) represents how close the cross-sectional shape of your muscle is to the
shape of a circle, where 1.00 is a circle and the lower the number, the better it is.
I’d never heard of that metric before. But the good news is that in this study, both
young and old people were able to decrease their SFI by the same amount over the study
period.
-
Not a link, but a nice quote:
Wrong decisions are part of life. Being able to make them work anyway is one of the abilities of those who are successful.
— Warren Buffett
I can’t seem to find things on the web as well as I used to. I blame Google being
enshittified, but
whatever the reason, I’m going to post links here. Not sure of the tempo or format but I
guess I’ll figure that out.
-
Lydiard Lacing. I’ve been having trouble with my toes and someone mentioned that
changing my lacing might help. I’ve tried Lydiard Lacing for a few weeks and it gives
my toes a lot more room. I fear that Nike link will
eventually rot, so here’s another explanation.
-
Big Three. Three exercises I’ve been doing for my back
-
RockAuto - An alternative to Amazon for car parts. I
needed wiper blades, so checked where reddit recommended to buy them
and also which brand to buy.
-
MediaCMS -
Someday I’d like to try this out for all the family photos and videos we have.
I just went down a Cory Doctorow rabbit hole. It started from a link in Austin Kleon’s newsletter to Doctorow’s post about his blog being his version of a commonplace book or a Memex. I remember Doctorow as being one of the early famous bloggers and an early crusader against unending copyright, but I haven’t really paid much attention to him since those early days. I distinctly remember when his first book, “Down and Out in the Magic Kingdom” was released for free on the internet. I remember it being surprising because he was “just a blogger” and now he was writing a real book. I was intrigued by some of the ideas in it. Like the concept of Whuffie, which was a social status indicator that everyone could see floating above your head, so that you knew who was important and who was a loser. With augmented reality, this might come true sooner than we think. I actually couldn’t initially remember the name of the book so I had to look through his book list to find it, and then saw that he’s written like 20 books now, many which look really interesting, so my to-read list just grew a bit. I also found his article about enshittification, which I think is one of the best essays I’ve seen in recent years. I’ve heard the term a lot, but didn’t realize that he had coined it. That article is another reason that I’ve started to write again, here on a page that I own.
I’m not sure that title is an exact quote, but I thought I heard Arthur Brooks say something like that as he was interviewed on a Peter Attia podcast. At least that’s what I took from whatever he said. His point was that the common advice to “follow your bliss” is misguided. When faced with choices, you shouldn’t choose the easy thing, you should choose the hard thing. I’m not sure that any of this is revolutionary, but that title sure is kinda surprising to me, and I think it makes a lot of sense.
What would have made me happy this evening? Certainly way low on that list is writing this blog post. As you can tell if you follow my blogging (ha!), I clearly don’t like to write in public. The easy thing, the thing that my brain was telling me to do because it promised me happiness, was to sit down and scroll through my phone, or pick up my Kindle and read a novel, or basically do anything that was not me trying to create something. The hard thing, the thing I knew would be painful, was to scribble down this post because I know it will never be as good as the post that is in my brain. Taking this idea in my brain, which is perfect because nobody else can see it, and trying to put it on the page here… well that is scary and painful and I know people will wonder why I’d even think this was worth thinking, let alone sharing with the world. But in the long run, doing this activity of taking ideas in my brain, and working with them on the page, especially in public is clearly going to be better for me than leaving them in my brain. It will lead to me being a happier person.
Doing the thing that won’t make me happy is the key to happiness.
Today, I have a guest post for you from a very famous author.
By: Avik Kurup
If you’re going to visit Italy, I believe that these three tips will make you have an amazing trip.
First and foremost, visit Florence, Rome, Venice, and Cinque Terre. Florence has delicious food and the best gelato out of all of these places. Rome has the best pizza. Also, the colosseum and the forum are important and fun sites to see there. In Venice they have incredible pasta and seafood and many places to ride on boats.
Another important thing to know about visiting Italy is that you don’t want to drive. Cars are difficult to use because there are a lot of one way roads and confusing traffic lights. You will enjoy walking or going on a bike tour more. You can also use the train for longer distances.
The last tip that will help you enjoy your trip to Italy is you should eat as much pizza, pasta, and gelato as possible. Pizza in Italy has a crunchier crust and they put a ton of cheese. When you order pasta the bowl is humongous, but there is a small hole in the middle that is filled with pasta. It is way more than you think. I recommend the pasta bolognese. Italian gelato is fresh and inexpensive. You can get two flavors in a cup for $2.50!
Clearly, Italy has fantastic sights to see and food to eat. If you follow these three tips you will have a great trip!
The problem
The USB-C cord kept falling out of my Android phone. It started happening in the car. A
little bump while driving would make the cord fall out. Then it started happening even
when I just had it plugged in on a table. I’d come down in the morning and the charge
would be drained because it hadn’t been fully plugged in. Finally, I couldn’t even get
it to charge unless I plugged it in forcefully, and put a book under the cord at a
certain angle to keep it plugged in.
The googling
Googling for this problem didn’t find anything specific to my phone, but I did find
people complaining of this issue and other people telling them that this was because of
lint in the USB-C port.
[1]
[2]
[3]
I just needed to get that lint out somehow.
What didn’t work
- Compressed air
- A toothpick (it was too thick)
- A plastic zip tie (It was too flimsy)
What did work
A SIM card removal tool. You know, one of those things that they send you with a new
phone to poke into the SIM card housing to get it to eject? It was the perfect size and
depth to be able to get all the way around the SIM card and get copious amounts of lint
(ewww!) out of the port. Now my USB-C cord plugs in with a satisfying click and stays
connected.
Philosophical musings
It’s weird that this three year old phone now feels new to me. For a while now, I would
have a little dread every time I went to plug in this phone, knowing that it would be
fiddly and that I might come down to a dead phone in the morning. Now, with this little
improvement, I feel a weird warmth towards the phone again, similar to that feeling I
had when it was a new phone. I cleaned out the lint a few weeks ago, and I still have
this warm sensation towards it. Every time I plug it in, I get a little burst of
happiness when it clicks in satisfyingly. It’s almost as if seeing a problem with the
phone that I didn’t think would exist, and then seeing a solution to that problem, makes
me appreciate the phone more than if it had never had that problem. That just feels
weird and revelatory to me.
I have a new favorite laptop. I needed
a new non-work laptop and Linux is my OS of choice. It has been for at least a decade,
but recently that favoritism has been cemented since I chose to use a Macbook Pro for
work. After 6 months with the Mac, I’m finally starting to feel productive with it, but
it has been a painful re-learning (and un-learning) process. I still fondly return to my
Linux machines at the end of the work day. Mac OS X is just too “in-your-face” for me.
So I started planning to get another ThinkPad when I heard about
frame.work on Hacker News. They are a startup focused on building
functional, modular, repairable laptops which are also beautiful, light and fun to
use. Check out their “About” page for more about their mission, but it resonated with
me. I’ve always loved pokeing around my
computers and it’s unfortunately gotten much harder to do that with all of my electronic
devices. Frame.work is fighting against that trend.
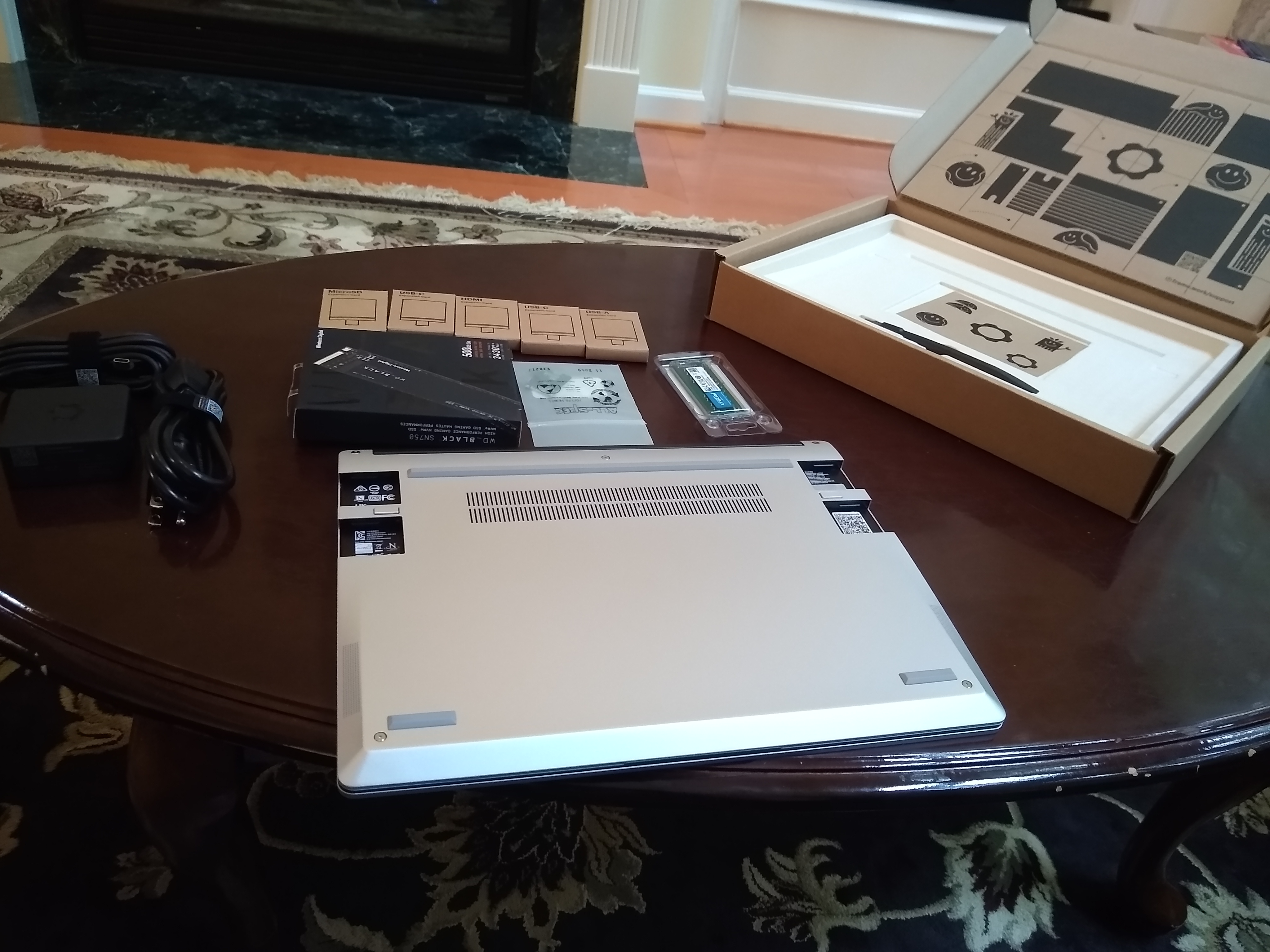
 Frame.work laptop contents
Frame.work laptop contents
They have a DIY option where you install your own RAM, SSD and WiFi module. Even the
non-DIY option comes in with external pluggable modules so you can configure your
accessories. I got 2 USB-C ports, a USB-A port, an HDMI-port, and an SD-card reader. But
it’s simple to pop out a module and pop in a new one. I don’t see myself doing that too
much, but when I do need that SD card reader, I’ll be smiling. Setting up the DIY parts was
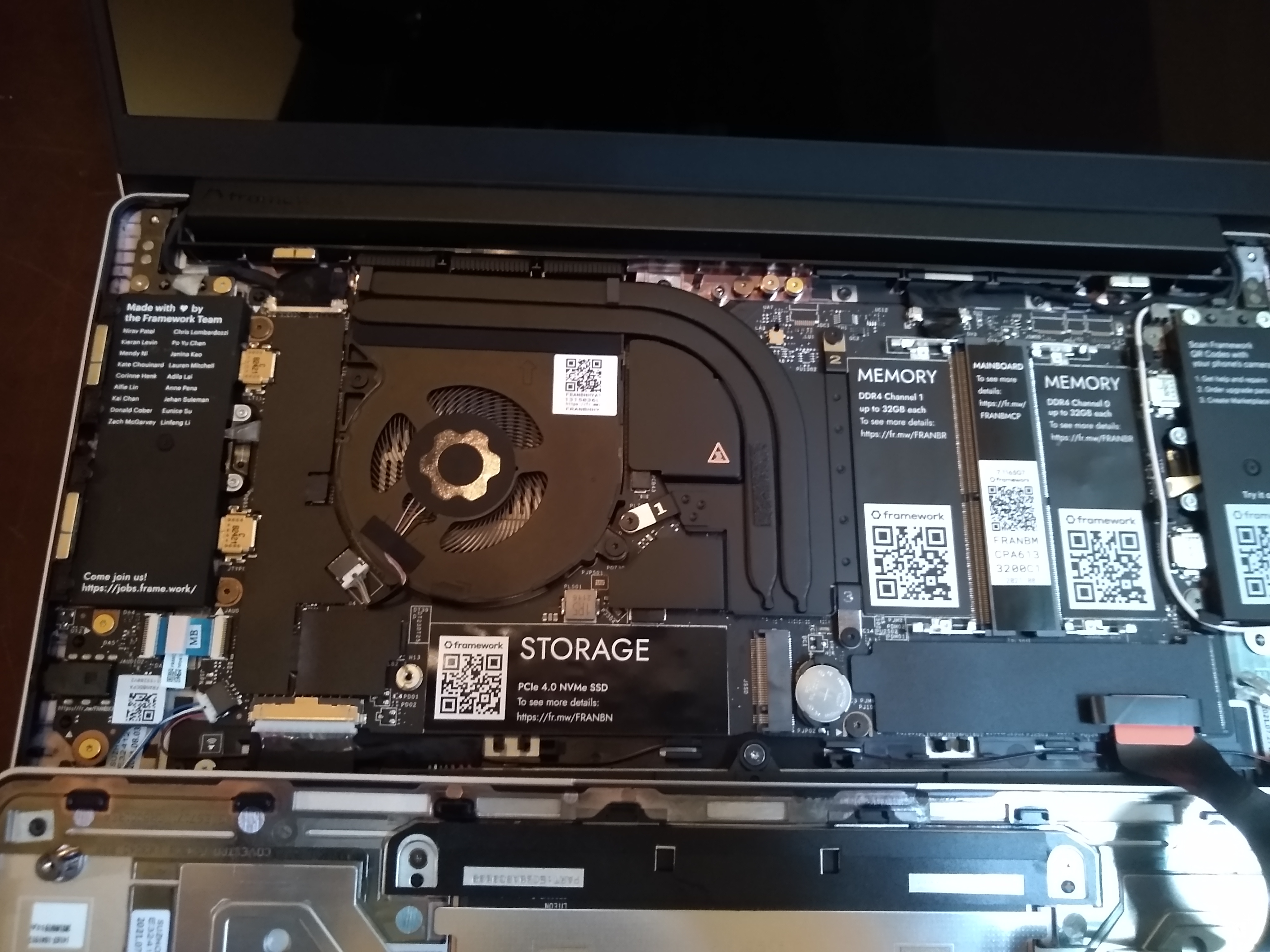
fun and easy. Each part has a QR code on the part and on the location in the laptop
where it gets installed, which points to detailed instructions.
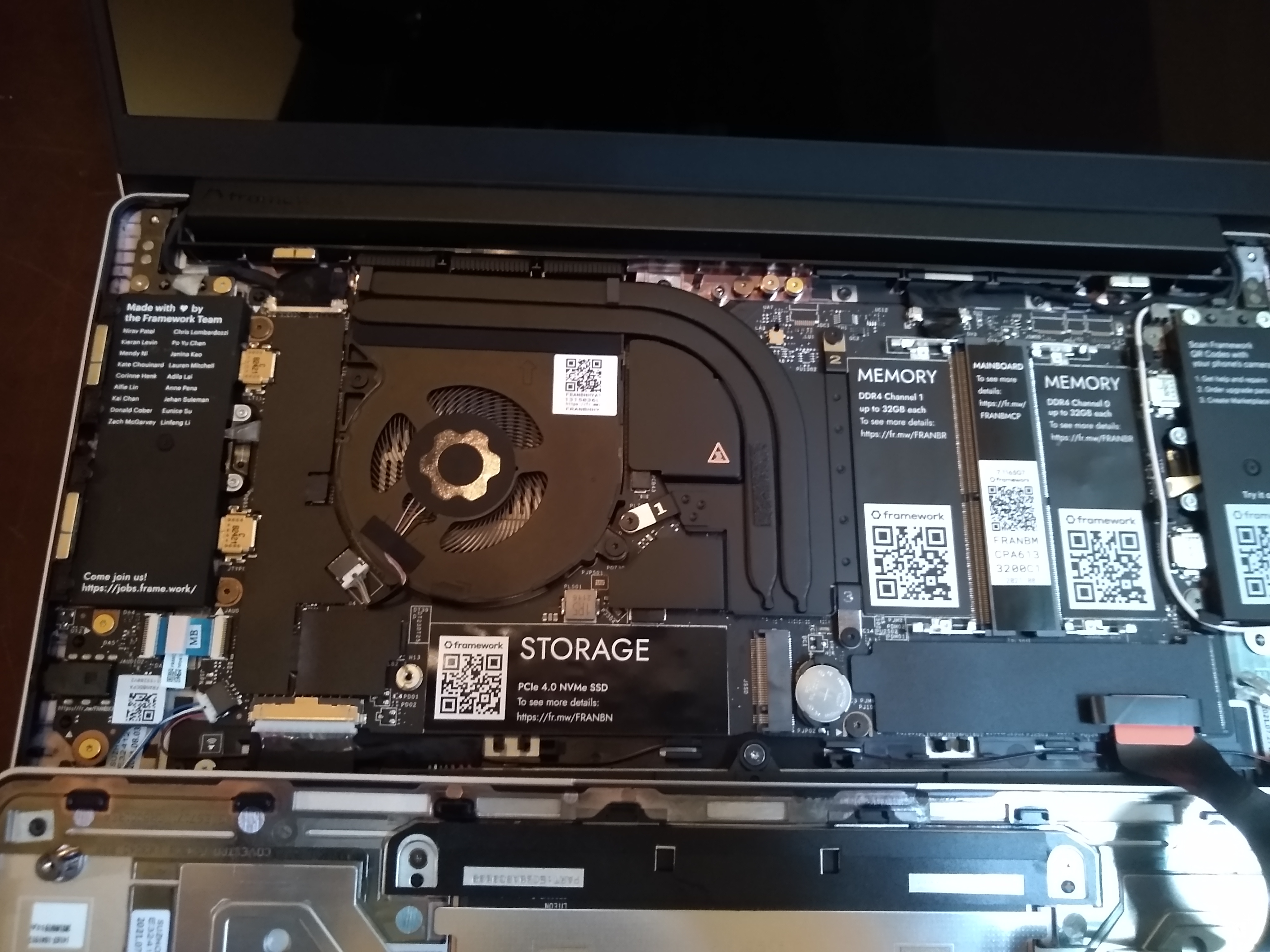 Frame.work laptop insides
Frame.work laptop insides
Ubuntu 20.04 doesn’t work out of the box (WiFi issues, I think?), so I installed 21.04,
and everything works except for the fingerprint reader (which never worked with Ubuntu
for me on my ThinkPad either). There are instructions to build the software needed to
get it to work, but I’ll wait for it to get rolled into a future OS release (I’m old).
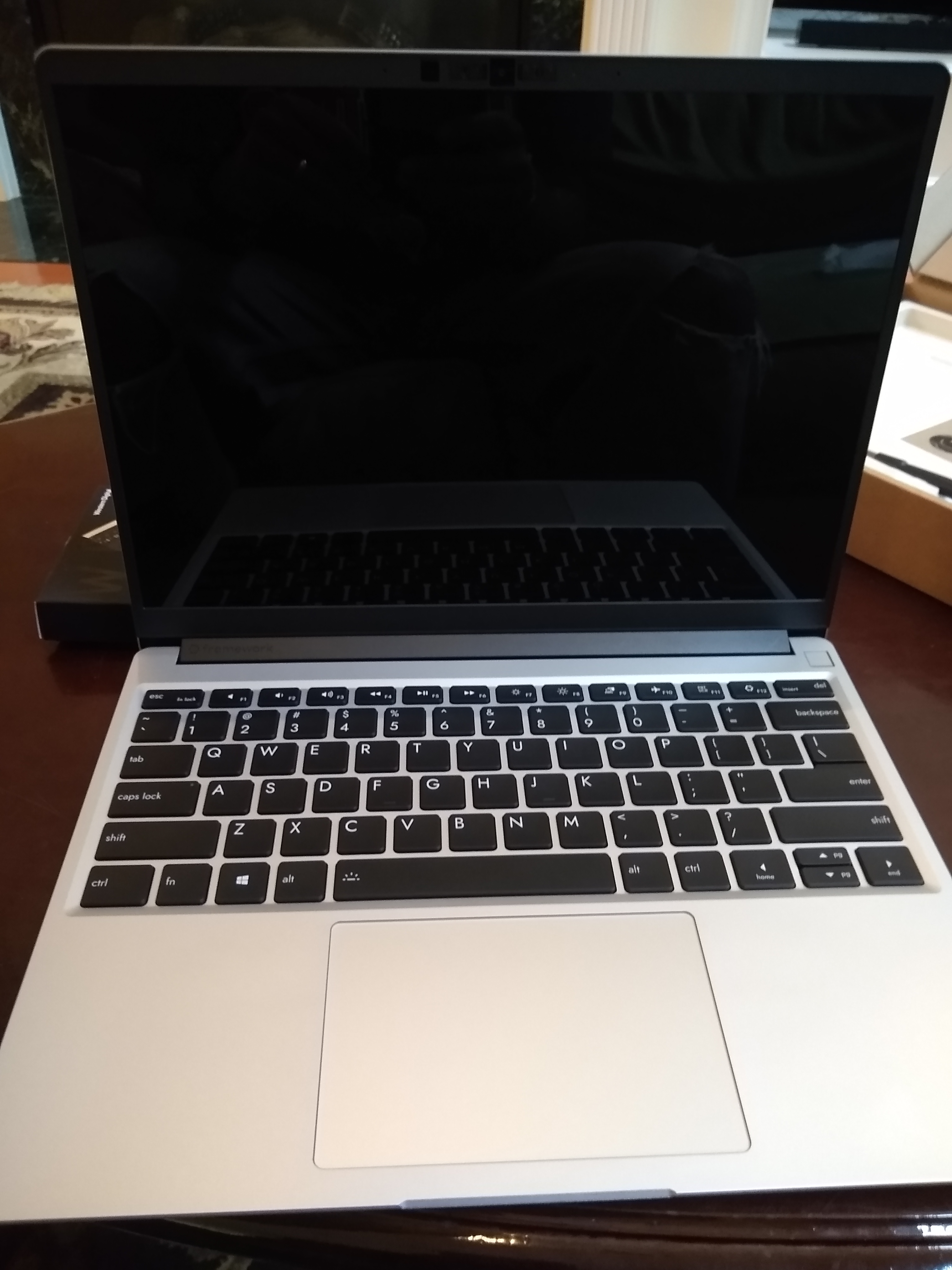
Overall, the computer itself is a dream. The screen is large and bright. The keyboard is
dreamy, compared to my Thinkpad X1 Carbon. I think it’s better than my MacBook Pro too,
but honestly that thing is too huge to use as a laptop so I always use it with an
external keyboard. The computer is light and the battery life is more than adequate for
my needs (though there are gripes and workarounds on the forums about this).
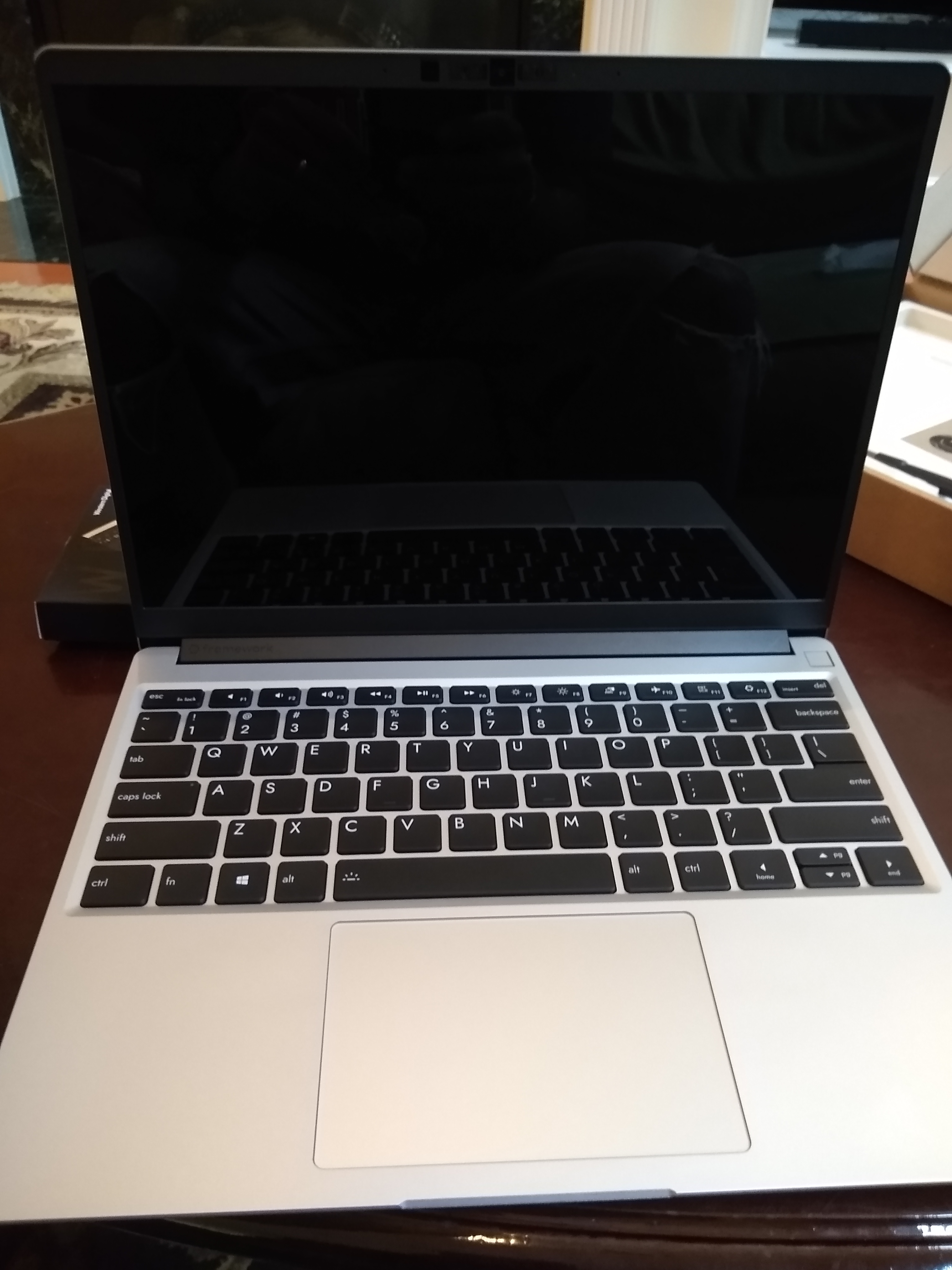 Frame.work laptop
Frame.work laptop
I thought that there would be more rough edges to the whole process, but I’ve been
pleasantly surprised. I hope others like it as much as I do so that the company sticks
around!